When the level of blood glucose, also called blood sugar, rises after a meal, the pancreas responds by releasing insulin into the bloodstream. Insulin helps cells throughout the body absorb glucose from the bloodstream and use it for energy.
Diabetes develops when the pancreas does not make enough insulin, the body's cells do not use insulin effectively, or both. As a result, glucose builds up in the blood instead of being absorbed by cells in the body.
In type 1 diabetes, the beta cells of the pancreas no longer make insulin because the body's immune system has attacked and destroyed them. The immune system protects people from infection by identifying and destroying bacteria, viruses, and other potentially harmful foreign substances. A person who has type 1 diabetes must take insulin daily to live.
Diabetes and Pancreatic Islet transplantation:
- Type 1 diabetes affects one in every 400 children and adolescents in the US.
- Pancreatic islets, also called islets of Langerhans, are tiny clusters of cells scattered throughout the pancreas.
- Pancreatic islets contain several types of cells, including beta cells, that produce the hormone insulin.
- Due to the limitations of exogenous insulin therapy and whole pancreas transplantation, pancreatic islet transplantation has emerged as a promising therapy for Type 1 Diabetes.
- Unsuccessful transplants can be attributed to several factors, researchers say. The current technique of injecting islets directly into the blood vessels in the liver causes approximately half of the cells to die due to exposure to blood clotting reactions.
- Also, the islets—metabolically active cells that require significant blood flow—have problems hooking up to blood vessels once in the body and die off over time.
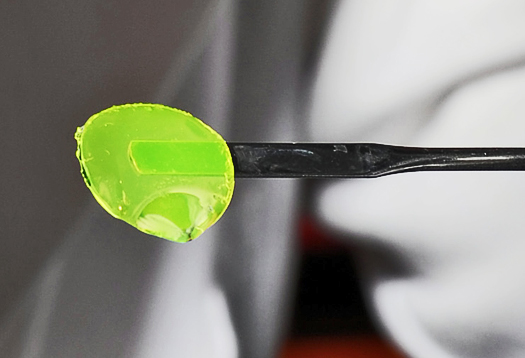
(Credit: Georgia Tech)
Georgia Tech and Emory University researchers engineered a hydrogel, a material compatible with biological tissues that is a promising therapeutic delivery vehicle. This water-swollen, cross-linked polymer surrounds the insulin-producing cells and protects them during injection.
The hydrogel containing the islets was delivered to a new injection site on the outside of the small intestine, thus avoiding direct injection into the blood stream.
Once in the body, the hydrogel degrades in a controlled fashion to release a growth factor protein that promotes blood vessel formation and connection of the transplanted islets to these new vessels. In the study, the blood vessels effectively grew into the biomaterial and successfully connected to the insulin-producing cells.
Four weeks after the transplantation, diabetic mice treated with the hydrogel had normal glucose levels, and the delivered islets were alive and vascularized to the same extent as islets in a healthy mouse pancreas.
The technique also required fewer islets than previous transplantation attempts, which may allow doctors to treat more patients with limited donor samples. Currently, donor cells from two to three cadavers are needed for one patient.

At Biotechnology Calendar, Inc. we produce life science shows at universities like Emory University, that allow for researchers like those working on breakthroughs in healthcare to discover new laboratory products and services. Take a look at the show gallery from last year's Emory Event and sign up to exhibit at our upcoming 16th annual BioResearch Product Faire™ event. Also, researchers, join us for free lunch, door prizes, and giveaways at the 2015 event.
Click the buttons below to see further funding statistics at Emory, or to exhibit at the upcoming BioResearch Product Faire™ Event on March 5th.