Ever since the 1940s, scientists, researchers, and medical professionals alike have been striving to understand why human bodies reject foreign objects, namely transplants. The first research to be done on this topic was by British researcher Peter Medawar during this time period, and for his founding of this scientific field of transplantation biology he received a Nobel Prize.
Since Peter Medawar's breakthrough research on tissue rejection, many efforts in the medical field have been made to reverse the body's often automatic rejection of organ transplants, such as those of the kidney, liver, and heart. With the growing success and popularity of organ transplants, there has been a new ray of hope for those with essential organs that are failing and have negative prognoses. However, despite the growing success of the actual transfer of organs between people, the one critical problem that has left the transplant receivers in a risky situation is their body's rejection of the foreign organ.

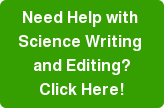
This image (courtesy of Lei Zhang of UW) shows the difference between two tissue samples post-implant. The first image on the left represents a thick collagen wall that has formed around a common material used for transplants. The image on the right represents the collagen dispersed evenly around a device implanted with this new hydrogel.
The human body's biological response to these foreign implanted devices is a very frustrating, and often successful, full-fledged attack on the transplant. First, the body formulates a protein wall (referred to as a collagen capsule) around the medical device, which isolates the device. This barrier is made of a protein, collagen, which is naturally occurring in the body, usually in the connective tissues (tendons and ligaments).
So far, scientists have yet to find a single material that has a reliable success rate for implants. With the first three weeks after a transplant being a very critical period for the patient, it becomes a waiting game for whether the patient will cut a lucky break and be able to use the organ for a period time, or more likely, the organ will begin show signs of a collagen wall build up and therefore have a very limited amount of time to use the organ before the body fully rejects the organ and the transplant is pronounced unsuccessful, usually leading to the death of the patient. Although physicians and scientists have found ways to lessen the destruction of the implanted organ, there has been no success in actually eliminating it.
That is, until now.
Thanks to the state-of-the-art research being done collaboratively at the University of Washington, a new material (a synthetic polymer), has been shown in mice to be undetectable by the body's biological defense system.
Shaoyi Jiang, a professor of chemical engineering at UW, remarks,
"Scientists have tried many materials, and with no exception, this is the first non-porous, synthetic substance demonstrating that no collagen capsule forms, which could have positive implications for implantable materials, tissue scaffolds and medical devices."
This unbelievable material, known as polycarboxybetaine methacrylate or PCBMA, is an improved hydrogel polymer substance. A hydrogel is a very malleable biomedical material that swells when introduced to water. This hydrogel comes from a polymer that has the capability to deflect all proteins from sticking to its surface.
The significance of this polymer is that it is the first of its kind to keep the destructive collagen capsules from forming in the first place. When proteins begin appearing around the medical implant, that is recognized as the first sign that a larger collagen wall will form and eventually isolate the device completely. However, even after three months of the polymer coated implants in the mice, there was no sign of any collagen walls of any kind, a very promising result considering the first few weeks after a human organ transplant are the most critical and usually can predict whether or not the body will attack the object or not.
The University of Washington researchers have been working in the modern field of transplantation biology for just shy of 20 years, searching for this type of miracle substance, a substance invisible to the body's natural immune response. This research effort really took off with the creation of the UW Engineered Biomaterials research center (UWEB) in 1996, funded by the National Science Foundation. Buddy Ratner (a UW professor of bioengineering and chemical engineering) took on the responsibility of director with his team, including Jiang, working very diligently on this product. And after two decades, they have something very impressive to show for their work, funded by the US Office of Naval research, UWEB, and the UW Department of Chemical Engineering. As perfectly stated by Ratner,
“This hydrogel is not just pretty good, it’s exceptional.”
These UW researchers have high hopes for what this polymer could mean for the future of organ transplants, and they plan to begin testing this in humans in the coming years by working with manufacturers to coat implantable devices with this polymer and subsequently test its effectiveness against the immune system's protein build-up defense.
If you are a life science researcher interested in learning about new laboratory research products for your research area attend Biotechnology Calendar, Inc.'s Seattle BioResearch Product Faire Front Line™ event at UW coming up on October 23,2013. Laboratory equipment suppliers are invited to showcase their products and network with top university researchers in a professional, popular trade show environment. This is BCI's 23rd annual show in Seattle on the University of Washington campus.
For a report with the latest UW research and funding statistics, click the button below.